I. Introduction
Oculomotor nerve palsy (ONP) makes up for one third of whole cranial nerve palsies1. It may result in ophthalmoplegia, ptosis or pupillary dilation, due to innervation of oculomotor nerve to levator palpebrae (LP), sphincter pupillae (SP), ciliary muscle, superior rectus (SR), inferior rectus (IR), medial rectus (MR) and inferior oblique (IO)2.
While several diseases are considered to be the causes of ONP3, there are strong likelihoods of midbrain or peri-mesencephalic lesions to be the cause, according to the nerve pathway. Somehow, post-stroke ONP has rarely been stressed in previous reports, contrast to dominantly studied traumatic, neoplastic or aneurysmal ONPs. As well, most traditional Korean medicine (TKM) studies about ONP are devoted to microvascular or idiopathic factors, but post-stroke ONP is rarely reported4-6.
Post-stroke ONP patients are much commonly found and difficult-to-treat than previously reported. Kim et al7 reported high prevalence and bad prognosis of post-stroke paralytic strabismus including ONP. Current conventional treatments are composed of managing risk factors, prescribing antiplatelets, occluding the affected eye, applying Fresnel prism or injecting botulinum toxin9. They are practiced in many cases but seem difficult to obtain satisfactory therapeutic outcomes. Surgical treatments are expensive, but they have risks of over-correction or under-correction. TKM treatments would be a great choice because they are more effective, low-cost and less harmful. More studies are demanded to make therapeutic advantages of TKM evident. We treated three post-stroke ONP patients with TKM therapies. One patient had subarachnoid hemorrhage (SAH) with non-recovery for 35 days after the onset and two patients had midbrain infarction lesions, all with severe initial ptosis and ophthalmoplegia. All of them had considerably good improvements, so we are reporting on them.
II. Case report
1. Case 1
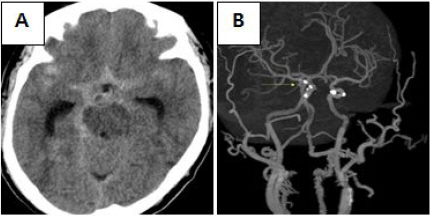
A woman with no significant past history, aged 61, a non-smoker who used to drink a bottle of beer every day, had lost her consciousness followed by a sudden, severe throbbing headache. Brain computed tomography (CT) and computed tomography angiography (CTA) showed an acute SAH, rupture of right anterior choroidal aneurysm, and unruptured PcoA aneurysm (Fig. 1). Right PcoA aneurysm clipping had been immediately gone through. 17 days later, recovering alertness, complete ptosis and ophthalmoplegia at right side of eye was revealed. She was transferred to our clinic after 35 days from the onset. Neurological examination revealed completely limited extraocular movement except for abduction, complete ptosis, horizontal nystagmus at left side gaze, all at the right side of eye and eyelid. Additionally, left side tongue deviation and both upper extremity intention tremor was present. Some steroids and anti-histamines were prescribed for rashes all over the body. Discharge medication from former hospital consisted of Levetiracetam 500 mg and Acetyl-L-Carnitine hydrochloride 590 mg, each to take twice a day. Electrocardiogram showed first degree arteriovenous block, but she had no related symptoms and vital signs were stable.
She was treated with a variety of herbal decoctions because of severe rash and fever, which was considered as drug allergy. Modified Buzhong Yiqi-tang, modified Yinqiao Baidusan, modified Shentong Zhuyu-tang, modified Wen Qing-yin, modified Banxia Baizhu Tianma-tang and modified Qinggan Mingmu-tang (Table 1), volume of 100 cc each, three times per day, were used until ptosis and ophthalmoplegia had fully recovered. The acupuncture treatment was performed at Jingming (BL1), Zanzhu (BL2), Tongziliao (GB1), Chengqi (ST1), Sibai (ST2), Yin-tang (EX-HN3), Yuyao (EX-HN4), Taiyang (EX-HN5), Hegu(LI4), Taichong (LR3), Baihui (GV20), twice a day.
Table 1
Herbal Decoctions, Administration Periods and Herbs Prescribed to Case 1, 2 and 3
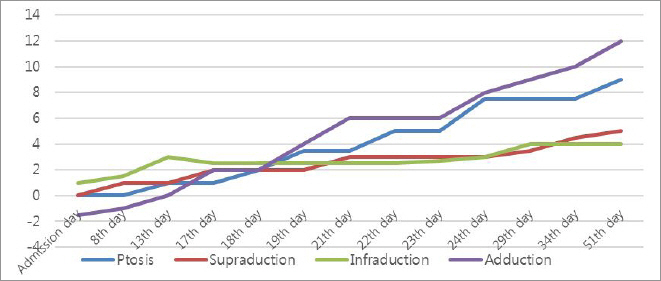
The effect of the treatment was evaluated by palpebral fissure (PF; the vertical height between the eyelids)8 and vertical and horizontal range of corneal light reflex from center to each margin of eyelids. At 51th day of admission, the chief symptom had vanished. PF improved from 0/9 mm to 9/9 mm. Range of corneal light reflex has also changed, elevation from 0/5 mm to 5/5 mm, depression from 1/4 mm to 4/4 mm, and adduction from -1.5/12 mm to 12/12 mm (Fig. 2, 3).
Fig. 1
Images of brain computed tomography, case 1. They were scanned on the onset of SAH. It shows an acute SAH (A) and aneurysm at right PcoA, 3.16 mm in size (B). The yellow arrow points at the aneurysm.
2. Case 2
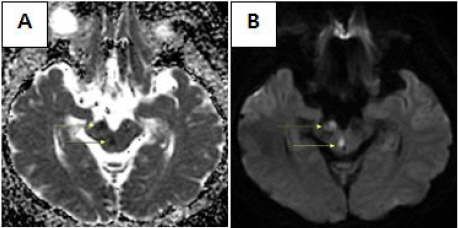
There was a 55-year old woman, with past medical history of hypertension and diabetes mellitus. She suddenly felt discomfort at keeping her right eye open, after suffering from dizziness for 2 days. As the ptosis progressed completely, she visited emergency room 3 hours later from the onset, and brain magnetic resonance imaging (MRI) scan revealed infarction at right midbrain (Fig. 4). Partial limitations of ipsilateral eye elevation, adduction and mild dysarthria were also found out by neurological examination. She had immediately received 100 mg of Aspirin every morning. On admission to our clinic, after a week from the onset, dizziness and ophthalmoplegia had disappeared but complete ptosis was still present. We prescribed her modified Buzhong Yiqi-tang (Table 1) for 20 days from admission to discharge. The acupuncture treatment was also performed at BL1, BL2, GB1, ST1, ST2, EX-HN3, EX-HN4, EX-HN5, LI4, LR3 and GV20 twice a day. PF was used as rating scale8, and it has improved from 0.5/8 mm to 2.5/8mm, by the time of discharge (20th day of admission) (Fig. 5, 6).
Fig. 4
Images of brain magnetic resonance imaging, case 2. They were scanned on the onset of brain infarction. ADC (apparent diffusion coefficient) (A), DWI (diffusion weighted imaging) (B). Yellow arrows point at the ischemic lesions of midbrain.
3. Case 3
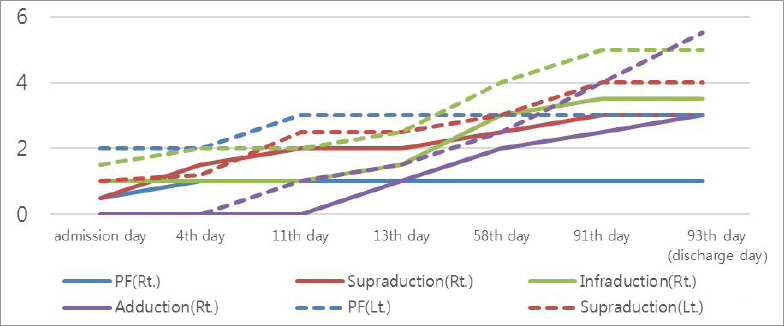
There was a 66-year old man, diagnosed with hyperlipidemia a year ago, who had been drinking one to three bottles of rice wine every day, for twenty-years. He fell asleep at pm 8:30, drunk as usual. Next morning, he woke up feeling weakness on his both legs. Stumbling to bathroom, suddenly lost consciousness so he was transferred to emergency room right away. The MRI scan showed multiple posterior infarction at both midbrain, left thalamus, right medulla, both posterior inferior cerebellar artery (PICA) territory and left superior cerebellar artery (SCA) territory (Fig. 7). CTA showed top of basilar artery (BA) occlusion, so the intra-arterial thrombolysis was conducted. Recovering his consciousness after few hours, he got his strength back but also recognized both of his droopy eyes. Atrial fibrillation was also revealed by transthoracic echocardiography, so doctors prescribed him Apixaban 2.5 mg twice daily. He was admitted to our clinic after a week from the onset. Neurological examination showed bilateral ptosis, loss of both light reflex, partial impairment of bilateral eye adduction, complete impairment of bilateral eye elevation and depression, pain in both eyeballs and left arm ataxia. He was prescribed with 100 cc of modified Buzhong Yiqi-tang for most part of his 3-month hospital stay, and modified Tongqiao Huoxue-tang for 10 days, 100 ml each, three times a day (Table 1). Medications containing anticoagulants, hypolipidemic agents were also continued. Acupuncture was also practiced two times a day, at BL1, BL2, GB1, ST1, ST2, EX-HN3, EX-HN4, EX-HN5, LI4, LR3 and GV20. PF and range of corneal light reflex from center to each margin of eyelids were also used as rating scale8. PF increased from 0.5/2 mm to 1/3 mm, elevation range of corneal light reflex from 0.5/1 mm to 3/4 mm, depression range of corneal light reflex from 1/1.5 mm to 3.5/5 mm and adduction range from 0/0 mm to 3/5.5 mm (Fig. 8, 9).
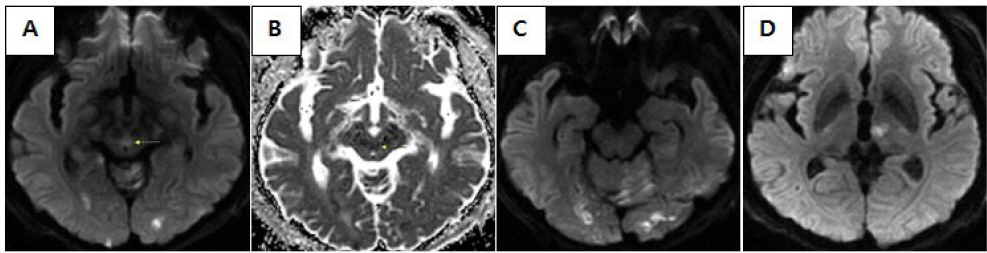
Fig. 7
Images of brain magnetic resonance imaging, case 3. They were scanned on the onset of infarction. DWI (A), ADC (B) showing acute infarction of both midbrain. DWI showing acute infarction of both ICA territory, left SCA territory, left PICA territory (C) and left thalamus (D). Yellow arrows point at the lesions of midbrain.
III. Discussion
Western medical treatments of ONP are focused on managing risk factors and prescribing antiplatelets9. They are important but insufficient to shorten therapeutic period and make better recovery. So additional therapies to make direct effects are demanded. Blurring lens of glasses with surgical semi-opaque tape or applying eye patch to the affected side are frequently used to relieve discomfort caused by diplopia. Fresnel prism can also be applied to realign the visual axis. Due to changing degree of misalignment in the recovery phase, various degrees of prisms are frequently required11. However, unilateral eye occlusion and prism therapies are just used to make adjustment to paretic condition, not to treat underlying ophthalmoplegia. Botulinum toxin injections to antagonist muscle of the affected eye are also used to resolve muscle contracture, but the effect only lasts for 3 to 6 months. Surgical treatment may be considered after follow up of 6 to 12 months11, because of its difficult process, risk of post-operative over-correction or under-correction10, and high risk of relapse11.
In TKM terms, ophthalmoplegia and diplopia can be explained as fengqian-pianshi (風牽偏視) or shiyi-weier (視一爲二). Ptosis can be explained as sangbao-xiachui (上胞下垂) or baochui (胞垂). The causes are categorized into stagnation of blood, deficiency of spleen, wet-phlegm obstruction, attack of wind or wind-heat, and wind of liver moving inside12. We also considered brain infarction or hemorrhage to be treated, as it is the original cause of our three cases. Stroke is symmetrical to zhongfeng (中風) in TKM. Fire-heat, wet-phelgm, qi deficiency, yin deficiency or blood stagnation are the possible causes13.
Many former studies have proposed herb decoction or acupuncture therapy to treat ONP. Jung et al4, Kim et al5, Jun et al6 and Kim et al14 suggested Buzhong Yiqi-tang as the therapy of ONP. All of them differentiated the symptoms as spleen-qi deficiency on the basis of the theory that eyelids are related to qi of spleen. Furthermore, as the cause of diplopia is regarded as liver-wind, herbs that eliminate liver-wind by nourishing liver-blood are frequently used12. Acupuncture is a method of moving vital Qi through the meridian system, by stimulating acupoints on the base of TKM categorization15. Additional studies have asserted the effectiveness of stimulating acupoints around the eye, Xingnao Kaiqiao technique (醒腦開竅法), scalp acupuncture, multi-needle shallow acupuncture, pharmacopuncture, electro acupuncture and fire-needling acupuncture. Especially, many studies have reported that stimulating acupoints around the eye would achieve good effect for treating the symptoms of ONP16. According to analysis of 33 studies about acupuncture treatment for ONP16, acupoints of BL1, BL2, ST2, TE23, Ex-HN5, LI4, GB14, ST36, GB20, and GB1 turned up to be the most frequently used acupoints. Attempt of more invasive acupuncture therapy, by direct stimulation of extraocular muscles, has also been done and has shown good improvement17.
The first patient’s ipsilateral ophthalmoplegia, including SR, implies fascicular lesion because the oculomotor nucleus has contralateral innervation to SR. Although PcoA aneurysm is the highest risk of isolated ONP among all the other aneurysms, it’s not relevant in this case. The aneurysm has to be at least 4mm to injure the nerve18, but the patient’s one was only 3mm in diameter. Also, ophthalmoplegia and ptosis lasted for 3 months after the elimination of the aneurysm. The patient’s symptoms lasted too long to be regarded as transient ischemic attack, and no ischemic lesions at the third nervous pathway were found by MRI scan. While there are several other causes that might cause the nerve damage after SAH, such as vasospasm, intracranial pressure elevation, or subarachnoid clot19, we suspected the blood clot in subarachnoid cistern to have induced the neuropathy. Severe hemorrhage at subarachnoid space, especially at right side of peri-mesencephalic cistern, was revealed by CT. In TKM, she was identified as blood-stasis type and attack of wind type due to severe, persisting ONP accompanied with nighttime aggravating rash. So, the medications were focused on eliminating stagnation of blood by diffusing and circulating blood. The original decoctions, containing forsythiae fructus (連翹) and lonicerae flos (金銀花), were focused on symptoms of drug fever. Carthami flos (紅花), cnidii rhizoma (川芎), angelicae pubescentis radix (獨活) to remove blood stagnation, and osterici radix (羌活), saposhnikovia radix (防風) to eliminate wind, were added to almost every decoctions she took. Her ONP symptoms resolved completely at 85th day of the onset and 51 th day of the admission to our hospital. Considering that it was a complete palsy and was too severe that there was no improvement at all before the Korean medical treatment was done, it is obvious that the treatment we performed was effective.
The second patient was diagnosed with fascicular-ONP, because her ptosis was ipsilateral. Usually, ptosis caused by midbrain lesions occur bilaterally because of the damage of central caudal nucleus, which innervates LP bilaterally2,20. In some exceptional cases, unilateral ptosis occurs with midbrain lesions, which the cause is considered as fascicular lesion of oculomotor nerve21. In this case, lesions were shown at midbrain and cerebral peduncle, where the fascicles are located. She was identified as spleen-qi deficiency, so modified Buzhong Yiqi-tang was prescribed to supplement qi of spleen. Persicae semen (桃仁), carthami flos (紅花), cnidii rhizoma (川芎) was also added to remove blood stagnation, considering the ischemic lesion.
The third patient had almost complete ptosis and ophthalmoplegia except for LR, at both eyes, which can explain lesions at both oculomotor nucleus. He was also diagnosed as spleen-qi deficiency, according to his swollen tongue and weak pulse, so was medicated with modified Buzhong Yiqi-tang. Trichosanthis fructus (瓜蔞仁) and cnidii rhizoma (川芎) were added to eliminate stagnation of Qi, phlegm and blood. Considering his irritating eyeballs, cassia semen (決明子), lycii fructus (枸杞子), chrysanthemi flos (甘菊) were supplemented, which cool liver fire and supply liver blood, resulting in alleviation of the eye function. As obstructions of cerebral vessels were severe, the improvements were slow compared to the first and second case. However, the ophthalmoplegia showed fairly good progress. Owing to diplopia, he couldn’t take even one step on the admission. But by the time of discharge, he was able to go anywhere he wanted assisted by walker and walk more than 30 steps by himself. He visited OPD continuously, and recovered both extraocular functions fully, 6 months after discharge.
In our study, the effects of TKM treatments including acupuncture and herbal decoctions on ONP were confirmed. Around-eye acupoints stimulation, which is reported to be effective and frequently practiced16, was common treatment for our three patients. It is thought to have made relaxation of extraocular muscle fascia and fibers, activated blood and lymph circulation22, resulting in recovery of ophthalmoplegia and ptosis. Also, all three patients were prescribed with Buzhong Yiqi-tang, which had been proved to have neuro-protective effect by antioxidation and anti-inflammatory effect23. First patient’s hemorrhagic lesion in subarachnoid cistern may cause neural damage or vasospasm-induced secondary ischemia by releasing oxyhemoglobin or endothelin2. Second and third patient had ischemic lesions, so lack of oxygen and glucose may also cause neural damage and inflammation2. The herbal treatments are thought to have alleviated the neurological symptoms by managing with neural damage and inflammation.
In conclusion, by measuring of PF and vertical & horizontal range of corneal light reflex from center to each margin, all three patients applied with TKM treatments had shown great improvement at ONP symptoms. It also has affected the quality of daily life, as dizziness and gait disturbance due to diplopia had resolved. They would be adequate choices to treat ONP according to its low side effect, low cost and more effective techniques compared to managing risk factors, antiplatelets, conservative treatments, botulinum toxin or operations. However, lack of studies about post-stroke ONP made it difficult to analyze exact therapeutic effect. As damage of central nervous system is usually long-lasting and leaves severe sequelae, more studies about prevalence, treatment rate, treatment period and therapeutic mechanisms of post-stroke ONP are required.