Randomized Controlled Clinical Trials of Warm Herbal Foot Bath Therapy for Insomnia: A Literature Review Based on the CNKI
불면증에 대한 한방 족욕요법의 무작위 대조군 임상연구 현황 : CNKI를 중심으로
Article information
Trans Abstract
Objectives:
This review investigated the research on warm herbal foot bath therapy (WHFT) for insomnia.
Methods:
A search was conducted on the China National Knowledge Infrastructure (CNKI) database to collect relevant studies published up to August 29, 2023. Randomized controlled trials (RCTs) comparing WHFT and sleeping pills in patients with insomnia were included. The methodological quality of the included studies was assessed using the Cochrane risk-of-bias assessment tool. The results of the meta-analysis were presented as risk ratios (RRs) or mean differences (MDs) and their 95% confidence intervals (CIs).
Results:
A total of 11 RCTs were included. WHFT as monotherapy resulted in a significantly higher total effective rate (TER) (RR, 1.25; 95% CI, 1.15 to 1.36; I2=25%) and an improved Pittsburgh Sleep Quality Index (PSQI) global sore (MD, -3.10; 95% CI, -4.24 to -1.95; I2=73%) compared to benzodiazepines. Additionally, WHFT as a combined therapy with benzodiazepines resulted in a significantly higher TER (RR, 1.15; 95% CI, 1.04 to 1.27; I2=0%) and an improved PSQI global score (MD, -2.23; 95% CI, -4.09 to -0.38; I2=80%) compared to benzodiazepines alone. In network analysis visualizing the components of HWFT, four clusters were discovered, and Polygoni Multiflori Ramuls and Ziziphi Spinosae Semen were the key herbs used in WHFT. Overall, the methodological quality of the included studies was poor.
Conclusions:
There was limited evidence that WHFT as a monotherapy or combined therapy was effective in improving insomnia. The findings can be used as basic data for future WHFT research in South Korea.
Abstract
초 록
목적:
이 연구의 목적은 불면증에 대한 한방 족욕요법의 연구 동향을 검토하는 것이다.
방법:
관련 연구의 수집을 위해 CNKI에서 검색을 수행하여, 2023년 8월 29일까지 발표된 연구를 검토하였다. 불면증 환자를 대상으로 한방 족욕요법과 수면제를 비교한 무작위 대조군 임상시험 만을 분석에 포함하였다. 포함된 연구들의 방법론적 질은 Cochrane risk-of-bias assessment tool을 사용하여 평가하였다. 메타분석의 결과는 위험비(risk ratios, RRs)와 평균차(mean differences, MDs) 및 그 95% 신뢰구간(confidence intervals, CIs)으로 제시되었다.
결과:
총 11편의 무작위 대조군 임상시험이 포함되었다. 분석 결과, 한방 족욕요법은 벤조디아제핀계 약물과 비교하여 유의하게 더 높은 총유효율(RR, 1.25; 95% CI, 1.15 to 1.36; I2=25%)과 개선된 피츠버그 수면의 질 지수(Pittsburgh Sleep Quality Index, PSQI) 총 점수(MD, -3.10; 95% CI, -4.24 to -1.95; I2=73%)를 보였다. 또한, 벤조디아제핀계 약물에 한방 족욕요법을 병용한 경우, 벤조디아제핀계 약물을 단독으로 사용한 것과 비교하여 유의하게 더 높은 총유효율(RR, 1.15; 95% CI, 1.04 to 1.27; I2=0%)과 개선된 PSQI 총 점수(MD, -2.23; 95% CI, -4.09 to -0.38; I2=80%)을 보였다. 네트워크 분석을 통해 한방 족욕요법에 포함된 약재를 분석하고 시각화한 결과, 4개의 클러스터가 발견되었으며, 핵심 약재는 야교등과 산조인이었다. 포함된 연구들의 방법론적 질은 전반적으로 낮았다.
결론:
이 연구는 불면증 개선에 있어서 단독요법 또는 병행치료로서의 한방 족욕요법이 효과적이라는 제한된 수준의 근거를 보여준다. 이 연구의 발견은 향후 한국에서 시행할 한방 족욕요법 연구의 기초자료로 활용될 수 있을 것이다.
I. Introduction
Approximately 10% of the adult population worldwide suffers from insomnia disorder, and this condition poses a significant public health burden1. The prevalence of insomnia in the elderly is especially high. According to a study conducted in Korea, 32.8% of the elderly over 60 years old suffer from insomnia disorder2. Insomnia disorder is a type of hyperarousal disorder experienced throughout the day and can be explained by both cognitive and physiological models of insomnia3. Among them, the cognitive model of insomnia serves as the theoretical basis for cognitive behavioral therapy for insomnia (CBT-I), an important non-pharmacological treatment for chronic insomnia4. Although this treatment is one of the most well-established treatments for chronic insomnia, due to limitations in accessibility, lack of knowledge, and lack of treatment motivation, CBT-I has been underutilized in clinical settings5. On the other hand, pharmacological treatment for chronic insomnia includes benzodiazepines and benzodiazepine receptor agonists, but their adverse side effects and lethal overdose have been pointed out6.
Therefore, it is important to discover non- pharmacological treatments that are effective for insomnia and highly available, and in this context, complementary and integrative medicine has received attention. According to the results of a network meta-analysis analyzing the comparative effectiveness of available non-pharmacological treatments for insomnia in the elderly, acupuncture alone or in combination with benzodiazepines was found to be effective in improving sleep quality7. In addition, a recently published multicenter, assessor-blinded, randomized controlled, pilot clinical trial found the effectiveness of electroacupuncture for cancer-related insomnia8. Given that it is difficult to challenge dysfunctional beliefs about sleep with acupuncture alone, as found in clinical trials comparing CBT-I and acupuncture9, the therapeutic mechanism of acupuncture is presumed to be primarily related to physiological models of insomnia3, including autonomic regulation10.
Another non-pharmacological treatment potentially involved in the physiological pathology of insomnia is foot baths. The effect of foot baths on improving sleep quality has been proven through some clinical trials11,12, and some of the mechanisms are thought to induce a relaxation response. In traditional East Asian medicine (TEAM), medicinal herbs have been used together with warm foot baths, namely herbal warm foot bath therapy (HWFT), to treat insomnia. HWFT is a kind of herbal external application, and an evidence-based clinical practice guideline published in China in 2012 recommended that herbal external application can be helpful for insomnia patients13. Some herbs may contribute to the treatment of insomnia through a synergistic effect when combined with a warm foot baths, but the additional clinical benefits of HWFT on the treatment of insomnia have not been reviewed. In South Korea, where TEAM, including herbal medicine, is frequently used, there has been no randomized controlled clinical studies (RCTs) investigating the effectiveness or efficacy of HWFT for insomnia. Therefore, this study aimed to investigate the current status of RCTs comparing HWFT and sleeping pills for insomnia, through a search in Chinese database.
II. Methods and materials
1. Search strategy
In this study, a search was conducted on China National Knowledge Infrastructure, a representative platform for Chinese research. The search was conducted on 29 August 2023, and all studies published up to the date of the search were reviewed. The search strategy was as follows: [subject] ‘herbal medicine’ AND [subject] ‘foot bath’ AND [subject] ‘insomnia’. The search was performed by one researcher (CYK).
2. Inclusion and exclusion criteria
The inclusion and exclusion criteria used in this study can be presented in the following PICOS format. 1) Population: Insomnia patient. There were no restrictions on the diagnostic criteria for insomnia and concomitant conditions. Also, there were no restrictions on sex/gender, age, or ethnicity of participants. 2) Intervention: HWFT. In this study, HWFT refers to warm foot bath therapy combined with herbs based on the principles of TEAM. As an intervention in the treatment group, HWFT was allowed to be used alone or in combination with sleeping pills. 3) Control: Benzodiazepines and benzodiazepine receptor agonists, which are standard drug treatments for chronic insomnia6, were allowed as controls. 4) Outcome: Studies reporting sleep-related outcomes were included. The primary outcome was the Pittsburgh Sleep Quality Index (PSQI)14, and other outcomes were considered to be secondary. 5) Study design: Only RCTs were accepted. Other study designs were excluded. Gray literature was allowed. There were no restrictions on publication language.
3. Study selection
Study selection was conducted by two independent researchers (CYK, BL) based on the inclusion criteria described above. Study selection was conducted in two steps. In the first step, titles and abstracts of documents were reviewed for potential relevance. In the second step, the full-text of the screened documents were carefully reviewed. Any disagreements between the researchers were resolved through discussion between them.
4. Data extraction
The following information was extracted from included studies using a predefined standardized Excel form: information for risk of bias assessment, country in which the study was conducted, publication language, sample size, mean age and sex ratio of participants, and pattern identification, materials and procedures of HWFT, outcome, results, and adverse events. Data extraction was conducted by two independent researchers (CYK, BL). Any disagreements between the researchers were resolved through discussion between them.
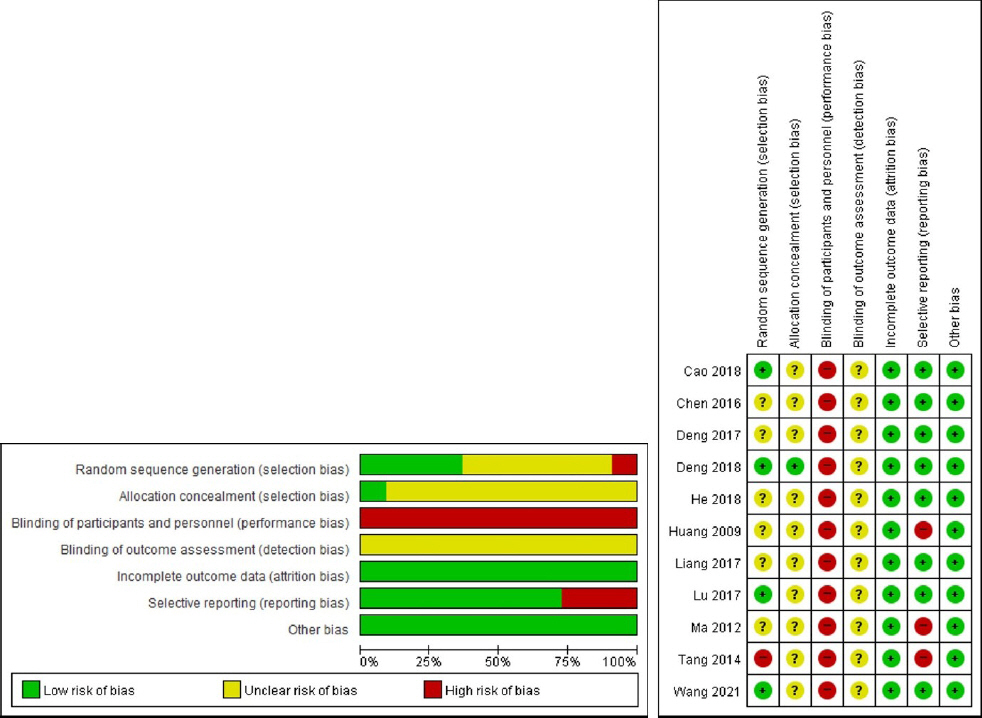
5. Assessment of methodological quality
The Cochrane risk-of-bias assessment tool15 was used to assess the methodological quality of included studies. Using the standard methodology of this assessment tool15, included studies were assessed. Using this tool, the risk of bias was assessed as low, high, or unclear for each of the following seven domains: random sequence generation, allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; selective reporting; and other sources of bias15. In case of other sources of bias, if the clinical equivalence of the treatment group and the control group at baseline was statistically reported, it was rated as low. Assessment of methodological quality was conducted by two independent researchers (CYK, BL). Any disagreements between the researchers were resolved through discussion between them.
6. Data analysis
All included studies were analyzed qualitatively. In addition, meta-analysis was conducted when two or more studies reported the same outcome. However, considering the potential heterogeneity of the HWFT used, the random-effect model was used in the meta-analysis. Meta-analyses for dichotomous variables were expressed as risk ratios (RRs) and their 95% confidence intervals (CIs), and meta-analyses for continuous variables were expressed as mean differences (MDs) and their 95% CIs. The I-square value was used to evaluate statistical heterogeneity, and if this value was greater than 50%, statistical heterogeneity was interpreted as significant16. Meta-analysis was conducted using Review Manager version 5.4 software (Cochrane, London, UK).
In this study, an analysis of the HWFT used was conducted. Specifically, the material, timing, duration, amount of liquid used, temperature (°C), treatment frequency, and treatment period were analyzed. In particular, herbs used in HWFT were analyzed by frequency, and their composition was clustered and visualized as a network using VOSviewer version 1.6.18 (Centre for Science and Technology Studies, Leiden University, Leiden, The Netherlands). In this network, the size of the nodes indicates the frequency of use of each herb, and the lines between nodes indicate the connectivity of the prescription composition between the herbs.
III. Results
1. Search results
Among the 233 initially searched documents, 204 irrelevant documents were excluded through the first step of screening. After reviewing the full-text of the remaining 29 documents, exclusion occurred for the following reasons: Combination treatment (but not sleeping pills) was used with HWFT (n=9), HWFT was used equally for both groups (n=1), not RCT (n=6); and sleeping pills were not used in the control group (n=2). Finally, 11 RCTs17-27 were included in this review (Fig. 1).
2. Characteristics of included studies
Included studies17-27 were published between 2009 and 2021. These studies were all conducted in China and published in Chinese. The sample sizes of these studies varied from 32 to 126, and the mean was 81.73. Except for one study24 that did not provide the average age of participants, the average age of participants in all remaining studies was over 40 years old. Nine studies17-19,21,23-27 recruited patients with primary insomnia, and the remaining two studies included comorbid conditions, including post-stroke insomnia20 and perimenopausal insomnia22. Eight studies17-19,21-24,27 compared HWFT with benzodiazepines, and other three studies20,25,26 compared HWFT combined with benzodiazepines and benzodiazepines alone. The treatment period varied from 7 to 90 days, with an average of 27.64 days. The most frequently reported outcome measure was total effective rate (TER) (n=10), followed by PSQI (n=7). The basic characteristics of the included studies are summarized in Table 1.
3. Methodological quality of included studies
Among the included studies, four studies21,24,26,27 were evaluated as low in the random sequence generation domain using randomization methods such as random number tables. One study19 was evaluated as high in this domain because it assigned treatment and control groups according to the order of hospitalization. In the remaining studies17,18,20,22,23,25, the methods were not described and were evaluated as unclear in this domain. Only one study26 described the allocation concealment method. Because the included studies were studies comparing HWFT and sleeping pills, double blinding was deemed impossible. There were no studies reporting blinding of outcome assessment. In the included studies, there were no or small number of participants dropping out, and the reasons were stated, so the studies were evaluated as low in the incomplete outcome data domain. In selective reporting, studies17-19 that reported only TER were evaluated as high because this outcome is not a validated evaluation tool for sleep disorders. Statistical equivalence between the two groups at baseline was reported in all studies, so all other sources of bias domains were rated as low (Fig. 2).
4. Methods of HWFT used in included studies
A total of 15 HWFT prescriptions were presented in the 11 included studies17-27. As a result of the analysis, 44 types of herbs were used a total of 113 times, and an average of 7.53 herbs were included per HWFT. As a result of frequency analysis of the medicinal herbs used, Polygoni Multiflori Ramuls (n=10) was most commonly used, followed by Zizyphi Spinosae Semen (n=8), Salviae Miltiorrhizae Radix (n=6), and Albizziae Cortex (n=6) (Table 2). Four major clusters could be established in the nodes consisting of each herb (resolution, 0.65; minimum cluster size, 1). The largest cluster was centered around Polygoni Multiflori Ramuls and Zizyphi Spinosae Semen. The second cluster was centered on Albizziae Cortex, Angelicae Gigantis Radix, and Bupleuri Radix. The third cluster was centered on Salviae Miltiorrhizae Radix. Lastly, the fourth cluster was centered on Ophiopogonis Radix (Fig. 3). In the nine studies18-25,27 that described the timing of HWFT, all included the timing at night or before bedtime. Most studies17,18,21-27 performed HWFT once a day, but one study20 performed HWFT four times a day and the other19 conducted HWFT twice a day. The optimal duration of HWFT per session was commonly 30 minutes. The optimal amount of liquid used for each HWFT was commonly 2.0-3.0 liters. When performing HWFT, the optimal temperature of the liquid was commonly 40-43 °C (Table 2).
5. Effectiveness and safety of HWFT on insomnia
All included studies were included in the meta- analysis. Meta-analysis was performed on TER, PSQI global score, and incidence of adverse events. According to the results, HWFT as monotherapy showed significantly higher TER (RR, 1.25; 95% CI, 1.15 to 1.36; I2=25%) and improved PSQI global sore (MD, -3.10; 95% CI, -4.24 to -1.95; I2=73%) compared to benzodiazepines (Fig. 4(a), (b)). Also, HWFT as combined therapy with benzodiazepines showed significantly higher TER (RR, 1.15; 95% CI, 1.04 to 1.27; I2=0%) and improved PSQI global sore (MD, -2.23; 95% CI, -4.09 to -0.38; I2=80%) compared to benzodiazepines alone (Fig. 5(a), (b)). A meta-analysis on the incidence of adverse events was possible in the comparison between HWFT and benzodiazepines. The results indicated that there was no significant difference on incidence of adverse events between HWFT and benzodiazepines groups (RR, 0.09; 95% CI, 0.01 to 1.07; I2=0%) (Fig. 4(c)). Deng26 compared incidence of adverse event between daily HWFT combined with estazolam 2 mg/d and estazolam 2 mg/d alone for 28 days. As a result, the HWFT group had statistically significantly lower incidence of adverse events (2/61 vs. 8/59, p<0.05).

Meta-analysis on HWFT as monotherapy: (a) total effective rate, (b) global score of the Pittsburgh sleep quality index, (c) incidence of adverse events.
HWFT : herbal warm foot bath therapy
IV. Discussion
This study was conducted to investigate trends in RCTs that investigated the therapeutic effect of HWFT in improving insomnia compared to sleeping pills. According to the results of analyzing the 11 included RCTs, HWFT showed a significantly higher TER and more improved PSQI compared to estazolam or diazepam as monotherapy or combination therapy for an average treatment period of about 1 month. The key herbs of HWFT for improving insomnia were Polygoni Multiflori Ramuls and Zizyphi Spinosae Semen. However, in addition to this, a cluster centered on Albizziae Cortex, a cluster centered on Salviae Miltiorrhizae Radix, and a cluster centered on Ophiopogonis Radix were identified. HWFT was recommended to be performed once a day for 30 minutes before bedtime, and is described to be performed at 40-43 °C with 2.0-3.0 liters of liquid. However, the methodological quality of the included studies was overall poor. In particular, due to the nature of HWFT and sleeping pills, blinding of participants and personnel was not possible. Moreover, assessor blinding was unclearly described in all studies.
Sleep is mediated by changes in core body temperature. When heat is dissipated from the peripheral part of the body, core body temperature decreases, which promotes drowsiness28. Warm foot bath increases peripheral blood flow without increasing core body temperature and transfers core heat to the peripheral region. It is thought that this will promote the loss of body temperature in the peripheral region, induce sleep onset, and improve sleep quality12. Foot bathing itself affects the activity of the autonomic nervous system, and especially promotes relaxation responses by increasing the activity of the parasympathetic nervous system29. In addition, warm foot bath can be combined with some herbs to improve skin permeability and increase the absorption rate of ingredients effective for insomnia30. It is possible that the aromatic volatiles of some herbs added to warm water may be absorbed by the patient’s nasal mucosa31. One study included in this review found increases in serum dopamine and serotonin associated with HWFT27. These research results suggest that HWFT has the potential to improve sleep not only through thermal stimulation but also through the biological effects of medicinal ingredients. However, there is a lack of research investigating the underlying mechanisms explaining the sleep improvement effect of HWFT. It is expected that future research in this field will be able to mimic research on foot baths using essential oils. For example, a study examining the effects of a foot bath using Lindera umbellate essential oil on individuals found that this foot bath increased parasympathetic nervous system activity and improved negative mood32.
Although there is a lack of evidence to clearly support the benefits of HWFT in the treatment of insomnia, this treatment has the advantage of being highly available and considered a safe non- pharmacological treatment. Compared to half-body baths, foot baths are considered safer and more beneficial as they gradually increase peripheral circulation33. In clinical practice, foot baths can be combined with foot reflexology and used synergistically to improve sleep34. In other words, given the importance of introducing non-pharmacological therapies in the treatment of insomnia, especially chronic insomnia6, HWFT is likely to be an attractive non-pharmacological option. More importantly, this treatment can also be used in patients who cannot or have difficulty using sleeping pills. However, there is still a lack of research investigating the sleep improvement effect of HWFT in South Korea, so related clinical research can be conducted considering the findings in this study.
The following limitations of this review are acknowledged. First, this study did not conduct a sufficiently comprehensive search, but mainly focused on collected studies of HWFT in traditional Chinese medicine, so there may be potentially relevant but missing studies. However, given that most research in this field is being conducted in China, we can roughly estimate the effect of HWFT on insomnia through the results of this study. Second, the methodological quality of the included studies is overall poor. This means that the reliability of the results obtained from these studies is challenged. Additionally, it is acknowledged that our findings may be significantly affected by the results of future rigorously conducted studies. Third, placebo effects may have played a role in the findings. The included studies were unable to be double-blinded due to the nature of the interventions, and some Chinese participants may have favored HWFT, a type of traditional Chinese medicine. Future studies could perform comparisons between HWFT and warm foot baths without herbs to better understand the effectiveness of HWFT on insomnia.
V. Conclusion
This study was conducted to investigate trends in RCTs that investigated the therapeutic effect of HWFT in improving insomnia compared to sleeping pills. HWFT showed a significantly higher TER and more improved PSQI compared to estazolam or diazepam as monotherapy or combination therapy for an average treatment period of about 1 month. There was limited evidence that HWFT as monotherapy or combined therapy was effective in improving insomnia. In this review, the composition and procedures of HWFT were analyzed in detail, which can be used as basic data for future HWFT research in South Korea.
Acknowledgement
This research was supported by the MSIT (Ministry of Science and ICT), Korea, under the Grand Information Technology Research Center support program (IITP-2023-2020-0-01791) supervised by the IITP (Institute for Information & communications Technology Planning & evaluation).