MARS-PD: Meridian Activation Remedy System for Parkinson’s Disease
Article information
Abstract
Objective:
There are currently no disease-modifying medications or definite long-term sustainable interventions for patients with Parkinson’s disease (PD), indicating an unmet treatment need. Our goal was to create a long-term sustainable intervention for PD patients that can be used in Korean medicine clinics.
Methods:
The Meridian Activation Remedy System (MARS) was created to stimulate a patient’s 12 meridians and sinew channels using a combination of acupoint stimulation and exercise. The acupoints and motions used in MARS were selected through literature studies and expert advice. The methodologies were refined using observational and case studies. With slow and fast movements, the MARS intervention was intended to activate both slow- and fast-twitch muscle fibers. Intradermal acupuncture and motion that shift the center of gravity were employed to enhance the patient’s balance and proprioception. In addition, the intervention included alternating movement exercises to address the complex cognitive decline commonly occurring in PD patients.
Results:
The following acupoints were chosen for the MARS intervention: bilateral Hegu (LI4), Houxi (SI3), Waiguan (TE5), Neiguan (PC6), Zhongchong (PC9), Yuji (LU10), Zusanli (ST36), Yanglingquan (GB34), Taichong (LR3), Kunlun (BL60), and Taixi (KI3). We also developed actions that can stimulate the body’s 12 meridians.
Conclusion:
We developed the MARS intervention, which combines acupuncture and exercise, to address the unmet therapeutic needs of PD patients. We hope that with additional research, the MARS intervention can be set as an effective therapeutic program for PD patients.
I. Introduction
Parkinson’s disease (PD) is the second most common progressive neurodegenerative disease, and its prevalence is growing with the world’s aging population and westernization1,2. PD has a slow pathological progression, and the patients’ systemic nervous systems, including the central, peripheral, and enteric nervous systems, are damaged many years before the disease manifests clinically3. Furthermore, due to decreased proprioception and balance, and an altered pattern of motor unit activation, PD patients suffer from a decrease in movement speed and muscle strength, resulting in complex problems such as loss and alteration of peripheral muscle function and composition4-6.
There is currently an unmet treatment need for PD patients as there are no disease-modifying medications or definite long-term sustainable interventions for PD7. As a result, long-term management and treatment methods for PD patients, as well as a medical system capable of effectively supporting them, are required. Evidence has recently accumulated that various exercise treatments may have disease-modifying effects when implemented in the mid-to-long term for Parkinson’s disease patients8. However, its application in clinical practice is insufficient as there are barriers for PD patients to exercise consistently, and there is currently a lack of a sustainable system that can efficiently and systematically support PD patients to engage in exercise9. As a result, it is necessary to develop a special therapeutic exercise method for PD patients that can be performed efficiently by medical personnel and is long-term sustainable. In that context, the authors developed an effective and easy-to-follow “Meridian Activation Remedy System (MARS)” for patients with Parkinson’s disease.
II. Methods
MARS was designed to stimulate the patient’s 12 meridians and sinew channels efficiently by combining acupoint stimulation and exercise. Specific acupoints and motions used in MARS were selected through expert advice from doctors of Korean Medicine and exercise physiology from September 2020 to February 2021, and the methodologies were further specified based on an observational study (yet to be published) and a case study10 conducted in 2021.
Through a review of the literature, the researchers noticed that slow-twitch muscle fiber hypertrophy and fast-twitch muscle fiber atrophy appeared in PD patients11. MARS intervention was designed to be performed with both slow movements at 30 bpm and fast movements at 120 bpm in order to evenly activate the patients’ slow-twitch muscle fibers and slow-twitch muscle fibers. Furthermore, numerous studies have confirmed the decline in proprioception in PD patients, as well as the difficulty in improving the patients’ proprioceptive sense with dopaminergic medications12. To activate the patients’ proprioceptive sense, we devised a method for developing a sense of balance by combining acupuncture with movement that changes the center of gravity. Finally, our experience showed that complex cognitive decline with alternating movements was common in PD patients13. As a result, we devised an exercise sequence with alternating movements to allow the patients to receive complex cognitive training while exercising.
III. Results
1. Acupoints
Acupoints were selected based on clinical experience, and the Korean Medicine Clinical Practice Guideline for Parkinson’s Disease14. The acupoints selected for MARS intervention were as follows: bilateral Hegu (LI4), Houxi (SI3), Waiguan (TE5), Neiguan (PC6), Zhongchong (PC9), Yuji (LU10), Zusanli (ST36), Yanglingquan (GB34), Taichong (LR3), Kunlun (BL60), and Taixi (KI3). The acupoints were intended to be stimulated using stainless steel intradermal needles by licensed Korean medicine doctors. Table 1 shows the details about the acupuncture intervention methods in accordance with the Standards for Reporting Interventions in Clinical Trials for Acupuncture (STRICTA).
2. Actions that stimulate the meridians on the back of the body
We developed workout sequences to activate the meridians on the back of the body in order to improve the respiratory and immune functions of PD patients. The patient should be instructed to thoroughly warm up their ankle, knee, hip, waist, shoulder, elbow, and wrist joints prior to the workout. The workout sequences and instructions to activate the lungs, large intestine, kidneys, and bladder meridians on the back of the body are as follows. It is recommended that each patient exercise the contralateral side first to adapt the body to the exercise, activate the muscles, and then exercise the affected side. The same method can be carried out for the rest of the action (Fig. 1-6).

Workout sequences for lung and large intestine meridians.
The patient is standing with both hands interlocked on the back of the head and the elbows opened as wide as possible. The patient is then instructed to rotate his or her torso to the right and left. It is recommended that each patient exercise the contralateral side first to adapt the body to the exercise, activate the muscles, and then exercise the affected side. The same method can be carried out for the rest of the action.

Workout sequences for kidney and bladder meridians.
The patient stands upright with both hands on a wall at chest height. The patient is instructed to lift one leg forward and then extend it backward, similar to a Taekwondo back kick.

Workout sequences for pericardium and triple energizer meridians.
Instruct the patient to take a saddle stance and straighten his or her upper body. Instruct the patient to stretch forward his or her both arms and guide the patient to alternately extend the fingertips outward and inward.

Workout sequences for liver and gallbladder meridians.
Instruct the patient to stand upright with his posture and upper body straightened. Instruct the patient to stretch his or her right and left legs forward one at a time, and to alternately extend his or her toes outward and inward. Instruct the patient to extend the leg as far as possible without bending the knee.
Workout sequences for heart and small intestine meridians.
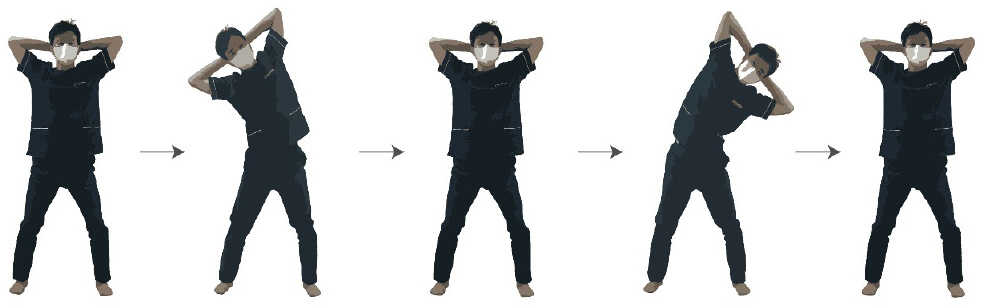
The patient is standing with both hands interlocked on the back of the head and the elbows opened as wide as possible. The patient is then instructed to alternately stretch his or her torso to the side, right, and left.

Workout sequences for pancreas and stomach meridians.
While standing upright, the patient is instructed to lift one leg forward and then extend it forward, similar to a Taekwondo front kick.
1) Lung and large intestine meridians
The patient is standing with both hands interlocked on the back of the head and the elbows opened as wide as possible. The patient is then instructed to rotate his or her torso to the right and left (Fig. 1). This movement should be repeated 10 times, slowly (10 reps at 30 bpm) and quickly (10 reps at 120 bpm).
2) Kidney and bladder meridians
The patient stands upright with both hands on a wall at chest height. The patient is instructed to lift one leg forward and then extend it backward, similar to a Taekwondo back kick (Fig. 2). This movement should be repeated 10 times, slowly (10 reps at 30 bpm) for the right and left legs, and then quickly (10 reps at 120 bpm) for the right and left legs.
3. Actions that stimulate the meridians on the side of the body
In order to stimulate the PD patient’s endocrine and autonomic nervous systems, we developed workout sequences to activate the meridians on the side of the body. The actions to activate the pericardium, triple energizer, liver, and gallbladder meridians on the side of the body are as follows.
1) Pericardium and triple energizer meridians
Instruct the patient to take a saddle stance and straighten his or her upper body. Instruct the patient to stretch forward his or her both arms and guide the patient to alternately extend the fingertips outward and inward (Fig. 3). This movement should be repeated 10 times, slowly (10 reps at 30 bpm) and quickly (10 reps at 120 bpm).
2) Liver and gallbladder meridians
Instruct the patient to stand upright with his posture and upper body straightened. Instruct the patient to stretch his or her right and left legs forward one at a time, and to alternately extend his or her toes outward and inward. Instruct the patient to extend the leg as far as possible without bending the knee (Fig. 4). This movement should be repeated 10 times, slowly (10 reps at 30 bpm) for the right and left legs, and then quickly (10 reps at 120 bpm) for the right and left legs.
4. Actions that stimulate the meridians on the front of the body
The purpose of activating the meridians on the front of the body was to stimulate the function of the patient’s gut-brain axis. The actions to activate the heart, small intestine, pancreas, and stomach meridians on the front of the body are as follows.
1) Heart and small intestine meridians
The patient is standing with both hands interlocked on the back of the head and the elbows opened as wide as possible. The patient is then instructed to alternately stretch his or her torso to the side, right, and left (Fig. 5). This movement should be repeated 10 times, slowly (10 reps at 30 bpm) and quickly (10 reps at 120 bpm).
2) Pancreas and stomach meridians
While standing upright, the patient is instructed to lift one leg forward and then extend it forward, similar to a Taekwondo front kick (Fig. 6). This movement should be repeated 10 times, slowly (10 reps at 30 bpm) for the right and left legs, and then quickly (10 reps at 120 bpm) for the right and left legs.
IV. Discussion
Patients with PD experience both motor symptoms such as slowness of movement, stiffness, tremor, and postural instability, as well as non-motor symptoms such as insomnia, constipation, and depression, which significantly impair the patient’s quality of life. Patients with PD have unmet needs for disease-modifying treatment7 as well as symptomatic treatment (i.e., improving the motor and non-motor symptoms of PD)15. As a result, we designed the MARS intervention as a personalized treatment program for individual PD patients with a variety of motor and non-motor symptoms. Through MARS intervention, we aimed to improve gait function, prevent falls, relieve stiffness and tremors in PD patients, as well as to improve non-motor symptoms such as constipation and insomnia. The following are some of the potential treatment mechanisms of MARS intervention for alleviating motor and non-motor symptoms in PD patients.
First, intradermal acupuncture stimulation combined with exercise sequences can boost the proprioceptive sensation of PD patients. The acupoints used for MARS intervention are chosen according to clinical practice guidelines for PD14 and are designed to stimulate 12 meridians evenly. When muscle contracts and moves, its proprioceptors send information about the movement to the central nervous system, which then issues another command to adjust the movement. The neurons of the globus pallidus of the basal ganglia respond 1:1 to the movements of the human joints and receive proprioceptive information. In PD, the degree of differentiation of the basal ganglia neural network including the globus pallidus is reduced, and neurons in the basal ganglia are excessively synchronized, making it difficult to process responses or movements related to a specific context. Furthermore, because of the increased noise in neural signals in the basal ganglia, controlling the premotor area becomes difficult. These are the suspected causes of bradykinesia. Furthermore, because the temporal resolution of the proprioception feedback loop is reduced, PD patients have decreased kinesthesia and postural instability13. Intradermal acupuncture stimulation was incorporated into the MARS intervention to increase the feedback strength of proprioceptor signals in the limbs. We postulated that it will be possible to strengthen the proprioceptive signals that enter the central nervous system as muscles move, allowing the motor program in the brains of Parkinson’s disease patients to function more smoothly.
Second, exercises that require both slow and rapid control of muscles can amplify the command that activates both the slow and fast twitch muscles. PD is associated with several skeletal muscle alterations, including hypertrophy of type I fibers and atrophy of type II fibers12, a modified pattern of motor unit activation11, a high root mean square (RMS), low heterogeneity between electromyogram (EMG) channels, particularly on the more severely affected side of the body16, and skeletal muscle transcriptional networks associated with type I myofiber grouping17. These alterations are associated with motor symptoms of PD such as bradykinesia and rigidity11,12,16. The MARS intervention is designed to start with slow movements at 30 bpm (beats per minute), followed by fast movements requiring precise and rapid control at 120 bpm. In other words, the goal of MARS intervention is to evenly activate commands related to slow-twitch and fast-twitch muscles. We believe that adequately activating slow-twitch muscles, which are hypertrophied in Parkinson’s disease patients, followed by activating fast-twitch muscles, which are at risk of atrophy, will improve motor ability while also promoting reinnervation and myofiber survival of type II fibers.
Third, acupuncture stimulation and exercise can alleviate pain in patients with PD. PD patients frequently complain of pain as a result of neuropathy, rigidity, and postural instability. Acupuncture stimulation is known to have an analgesic effect by increasing adenosine in the targeted tissue18. Exercise can promote circulation, enhance muscle strength, balance and postural stability, and increase flexibility in PD patients19. Therefore, a treatment combining acupuncture and exercise has the potential to relieve pain in PD patients.
Fourth, MARS intervention, which combines acupuncture stimulation and exercise, can prevent the decline of motor learning ability caused by Parkinson’s disease progression and activate brain plasticity. Acupuncture stimulates the motor cortex, which can aid in the restoration of the plasticity of the motor and cognitive neural networks. It is hoped that this will compensate for the loss of motor learning ability caused by problems in the basal ganglia circuitry. Jang et al. suggested that acupuncture can enhance gait and ameliorate the Unified Parkinson’s Disease Rating Scale (UPDRS) score as well as increase oxyhemoglobin levels in the prefrontal and supplementary motor areas while walking on a treadmill20. Furthermore, Chae et al. pointed out that stimulation of acupoint GB34 led to significant improvement in motor function as well as the activation of the putamen and the primary motor cortex in PD patients21. Therefore, we included the acupoint GB34 in the MARS intervention. Furthermore, we believe that combining acupuncture stimulation with exercise will improve the effectiveness of exercise treatment.
Lastly, MARS intervention has the advantage of being able to be developed as a customized program that more effectively alleviates various non-motor symptoms of patients by identifying the problematic meridian and providing intensive treatment to the affected area based on the patient. Along with motor symptoms, patients with Parkinson’s disease report non-motor symptoms such as dysphagia, constipation, insomnia, and restless legs syndrome22. The range of non-motor symptoms that patients report varies, and drug treatment cannot completely alleviate them. Therefore, it is necessary to address this issue by developing a patient-specific treatment plan. For example, in the case of a patient complaining of dysphagia and chest discomfort, upper extremity exercises combined with thoracic breathing training and stimulation of the acupoints of the lung meridian can be considered. Likewise, for patients with severe constipation, lower extremity exercises combined with abdominal breathing and stimulation of the acupoints of the stomach and large intestine meridians can be considered. For patients complaining of insomnia and restless legs syndrome, relaxation training combined with heart rate variability biofeedback and stimulation of the acupuncture point of the liver and heart meridians can be considered.
Qigong therapy, which is addressed in the Clinical Practice Guideline for Parkinson’s disease, is not performed in parallel with intradermal acupuncture and usually consists of slow movements. On the other hand, MARS intervention is different in that it is a compound exercise that utilizes both fast and slow beats for the purpose of evenly activating both fast-twitch and slow-twitch muscle fibers. For reference, for patients who cannot keep up with 120 bpm because it is too fast, the beat can be reduced to 110 bpm or 100 bpm. MARS is also distinct from Qigong therapy in that it mostly employs linear motions. MARS exercise can be easily modified to be performed in a sitting or lying position. As a result, patients with Hoehn and Yahr stage 3 or higher may benefit from the intervention as well. Meanwhile, the effect of MARS on non-motor symptoms of PD needs to be proven through future clinical studies.
V. Conclusion
There are currently unmet needs in PD patients for therapeutic exercise programs10. Furthermore, there are unmet needs for optimizing symptomatic control of both motor and non-motor symptoms of PD15. As a result, we developed the MARS intervention, which combines acupuncture and exercise to manage both motor and non-motor symptoms in PD patients. Although several studies show that exercise has a potential disease-modifying effect on PD, it has been reported that getting patients to continue exercising after completing a training intervention is challenging. As a consequence, there is a need for specialized clinicians to provide ongoing exercise programs for PD patients. We hope that in the future, MARS intervention can be further developed as a convenient and effective therapeutic program for PD patients. Further research is warranted to examine the efficacy and safety of MARS intervention.
Acknowledgments
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (Grant number: HF20C0174).
