I. Introduction
Bowel perforation is the formation of a hole in the wall of the gastrointestinal tract1. Bowel perforation is a disease that requires emergency treatment because substances in the gastrointestinal tract and intestinal bacteria can penetrate the abdominal cavity and lead to peritonitis2. The reason for the perforation in the intestine is that diseases such as colon obstruction, gastrointestinal cancer, gastric ulcer, and inflammatory bowel disease worsen, and it can also occur directly due to trauma such as a colonoscopy or cut by a knife3.
The main symptoms of bowel perforation are abdominal pain and tenderness. In case of perforation in the stomach or small intestine, the patient complains of sudden abdominal pain. In addition, when perforation occurs in the large intestine, abdominal pain may appear gradually. Symptoms other than abdominal pain include chills, fever, nausea, and vomiting4.
In general, emergency surgery is required for Bowel perforation. Therefore, sepsis can be prevented by suturing the hole using exploratory laparotomy and treating peritonitis by removing foreign substances that have flowed into the abdominal cavity1.
Therefore, in the treatment of patients with Bowel perforation, the key goal is to prevent complications by fast fusion of the perforations.
In this case, the author reports the improvement of the bowel perforation around ileo-anal anastomosis patient after the treatment with Korean traditional medicine due to the difficulty of surgical treatment caused by total colectomy.
II. Case
For the sutdy of this case, the patient signed conset form and IRB (Institutional Review Board) review exemption (DJDSKH-22-E-21) was approved by Daejeon Korean Medicine Hospital of Dae-Jeon University IRB.
1. Diagnosis and Patient symptoms
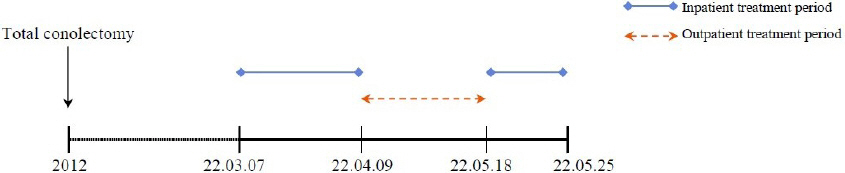
In March, 2022, a 42 year old male, visited the D University Korean Medicine Hospital for treating bowel perforation and recived two inpatient treatments and and one outpatient treatment for 76 days (Fig. 1). The patient had never been receiving any treatment since being diagnosed with perforation at a General Hospital in Ferburary, 2022. The perforation was discovered during regular follow ups for total colonectomy which was done because of colon polyposis in 2012. The reason for the perforation was untraceable, and it was discovered around ileo-anal anastomosis and pre-sacral space without transudate.
He heard from the his attending physician that it had difficulty to perform additioanl operation sealing perforation off since total colonectomy had already been performed. As performing a perforation surgery would be difficult, his primary physician suggested administering oral medication and monitoring him. Besides, the patient himself showed reluctance to operation. So, there were no additional alternatives. He was eager to receive Korean medicine treatment with a full understanding of the potential complications, such as peritonitis, and we started treatment.
A since several days before his first admission, he complained of a abdominal pain with a cramping and bloating and diarrhea worsened and was unable to carry out everyday life.
His blood pressure was 126/83 mmHg, pulse 79 times/min, respiratory rate 20 times/min, and body temperature 36.1 °C (Fig. 1).
2. Treatment and progress
Manual acupuncture treatment was performed twice a day during inpatient treatment period, and 3-4 times per week during outpatient treatment period based on the Korean medicine theory. Acupunture treatment was used by stainless steel needles in a thickness of 0.20 mm and a length of 15 mm (Dongbang Medical, Republic of Korea). The acupoints used were: LU07 (列缺, Lieque), KI06 (照海, Zhaohai), ST36 (足三里, Zusanli), LI02 (二間, Erjian), LI03 (三間, Sanjian), LI04 (合谷, Hegu), ST34 (梁丘, Liangqiu). 70 cc of Gami-Gamchogungang-tang (Jiawei-Gancaoganjiang-tang) was given to drink three times a day after meals. Normally, the patient was allowed to consume a soft diet, but when severe abdominal pain occurred, fasting was initiated, and total parenteral nutrition was carried out. His usual treatment of Ibuprofen Arginine 368.9 mg tid, Loperamide hydrochloride 2 mg tid were given to him until until the 20th day of treatment (Table 1).
Table 1
Prescription of Gami-Gamchogungang-tang (Jiawei-Gancaoganjiang-tang)
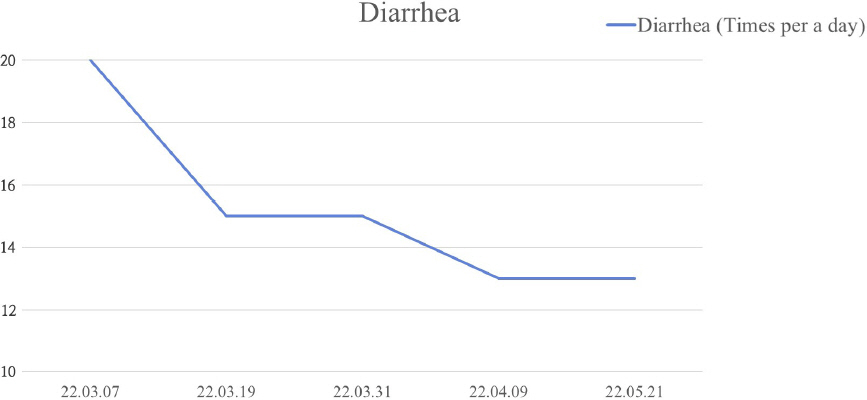
The treatment was assessed by comparing degree of abdominal pain, checking the frequency of diarrhea, biochemical tests, abdominal computed tomography (CT) and abdominal X-ray. Numeral rating scale was used as method to objectify symptom severity. Abdominal pain improved from NRS 5 on the first day of treatment to NRS1-2 on the last day of first inpatient treatment period. During outpatient treatment, the intensity of abdominal pain remained unchanged. At first day of second inpatient treatment day, the patient complained of abdominal pain on NRS 7, and it improved with NRS 1 on the last day of treatment. He had diarrhea 20 times per day on the first day of inpatient treatment, March 7th, 2022. The frequency of diarrhea on March 31st, 2022 was 15 times per day. On May 21st, 2022 at the end of the treatment, the number of diarrhea decreased to 13 times per day (Fig. 2, 3).
Fig. 2
Changes of numeric rating scale (NRS) on abdominal pain.
NRS of Abdominal pain decreased from 5 to 1.
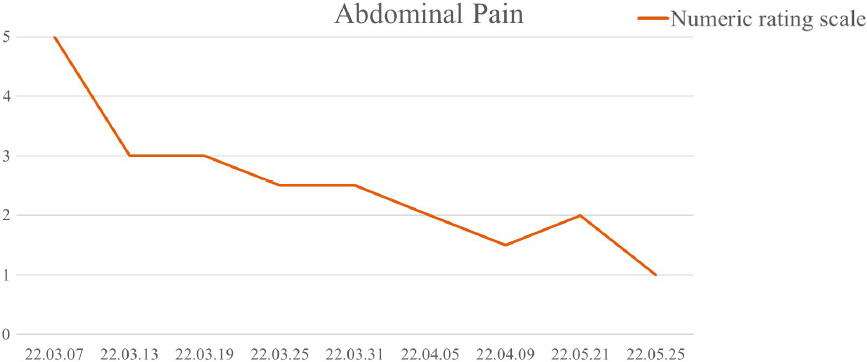
Fig. 3
Changes in the frequency of diarrhea.
The number of diarrhea decreased from 20 times to 13 times per a day.
Biochemical tests results were mostly normal, but there were abnomarlity in CRP (C-reactive protein). Results showed a CRP of 1.07 on March 8th, 2022. and 3.2 on May 19th, 2022. At the ends of the each inpatient treatment peroid, CRP levels were back to normal showed a CRP of 0.08 on March 28th, 2022, 0.45 on May 24 th, 2022 (Table 2).
Table 2
Laboratory Findings
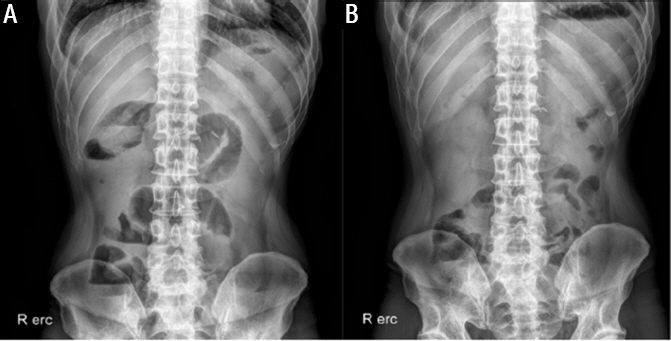
Abdomen CT showed branching patterned fistulas with inflammatory infiltration around ileo anal anastomosis and pre sacral space on February 16 th, 2022, and no specific foundings related to fisulas on May 21st, 2022 (Fig. 4). On abdminal x-ray taken on March 23rd, 2022, multiple air fluid levels in midabdomen were observed, and it was presumed to be a distal small obstruction. But, there were no significant abnormal gas pattern on abdominal x-ray taken on April 8th, 2022 (Fig. 5).
Fig. 4
Comparison of abdominal computed tomography.
A : Air containing, amorphic, branching patterned fistulas with inflammatory infiltration around ileo-anal anastomosis and pre-sacral space suggesting seal off perforation with fistula formation (22.02.16).
B : No Specific Findings Related with Fistula in the Abdomen Cavitiy (22.05.21).

Fig. 5
Compraison of abdominal x-ray (erect).
A : Multiple air fluid levels in midabdomen; distal small bowel obstruction (22.03.23).
B : No significant abnormal gas pattern. no definite noted ileus sign (22.04.08).
To tests for toxicity and side effects, Aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP) and Gamma- glutamyl transferase (GGT), typical liver funcion biochemical test, remained within normal range. Also, blood urea nitrogen (BUN) and creatinine, representing kidney function biochemical test, were no abnormal during treatments period. In order to assess the possibility of disease exacerbation, vital signs were checked in addition to blood tests, and there were no significant changes in body temperature or blood pressure. And, there were no unusal symptoms that the patient revealed.
III. Discussion
Statistically, it is reported that acute abdominal pain accounts for about 40% of all emergency surgeries performed in hospitals. Also, most cases correspond to secondary symptoms caused by fistula or Bowel perforation1. Intestinal perforation is a disease that requires emergency treatment because it can develop into peritonitis due to the penetration of substances in the gastrointestinal tract and intestinal bacteria into the abdominal cavity.
Bowel perforation treatment requires not only emergency surgery but also antibiotics and nutrition. The most important therapy for the treatment of Bowel perforation is by far source control. Source control is usually achieved by surgery. Surgery is performed to control the degree of damage, and the ultimate goal is to remove, clean, and regenerate the damaged intestine5,6. Therefore, source control is direct. It must be made to re-function the functional anatomy through the removal of inflammation, removal of contaminants in the abdominal cavity, and drainage of abscesses5. Antibiotics have become a standard treatment technique for treating the perforation of the gastrointestinal tract. Antibiotics are selected according to the site of the perforation7. Antimicrobial therapy is commonly used as an adjuvant treatment to prevent secondary peritonitis caused by perforation. Secondary peritonitis causes local inflammation and may cause complications such as bacteremia and sepsis5,7.
In Korean medicine, Bowel perforation belongs to the classification of 腸癰 (a localized pyogenic inflammation of the intestine) and 腹痛 (abdominal pain). We report this case because of the lack of studies previously reported on oriental medicine alone for the treatment of intestinal perforation. In this case, the patient came to our hospital to treat abdominal pain and perforation that occurred after follow ups for total colectomy for polyps of the colon. In this case, the patient started treatment at the hospital from March, 2022 with bowel perforation confirmed in February, 2022. Korean medicine treatment consisted of acupuncture treatment and herbal medicine treatment.
During the acupuncture treatment for perforation, the acupoints was performed as follows. LU07 (列缺, Lieque), KI06 (照海, Zhaohai). These acupoints were used not only for chest and abdominal pain but also obstetrics and gynecological diseases and digestive system diseases8. The combination of these two acupoints is used in common intestinal disorders. In addition, LI02 (二間, Erjian) has the effect of removing inflammation of the large intestine meridian9. ST36 (足三里, Zusanli) is the a acupoint of the stomach meridian and has the effect of treating inflammation of the intestine10. LI04 (合谷, Hegu) is the source of the blood of the large intestine meridian among the twelve meridians, and it is used for digestive system symptoms such as diarrhea and indigestion11.
The patient received Gami-Gamchogungang-tang as a basic prescription for Korean medicine treatment. Gamchogungang-tang, which has effects for treating external and interal Yin pattern, is recorded in a traditional Chinese medical text Shang Han Lun (On Cold Damage). When using the traditional Chinese medicine diagnostic tool, pulse diagnosis and tongue diagnosis, the pulse was tense and the tongue color was pale-rose, which indicate coldness. When we pressed on the abdomen, there was a feeling of abdominal distension, no rebound tenderness apeared, and the tender points were not consistent, with the pain moving around. Besides, he generally felt the abdominal pain like squeezing and cramping. Based on symptoms and these diagnostic tools, we diagnosed it as interior cold pattern, and we prescribed Gami-Gamchogungang-tang as the treatment for it. Cervi Pantotrichum Cornu, well known Yang-invigorating agent, was added to Gamchogunga-tang for the purpose of regaining and resuscitating energy (回陽, huiyang)12. It has been reported that Leejung-tang, derived composition with Gami- Gamchogungang-tang, is used to treat abdominal pain, and it has an anti-inflammatory function by affecting the production of cytokine secretion in the macrophages13,14.
During the outpatient treatment period, the treatment for perforation was continued through acupuncture and herbal medicine. In the case of hospitalization, both cases were abdominal pain caused by idiopathy, and abdomen X-ray showed ileus. At the time of hospitalization, in addition to the acupoints adopted at the time of perforation, two acupoints were collected from LI03 (三間, Sanjian) and ST34 (梁丘, Liangqiu) to solve the symptoms of indigestion. LI03 (三間, Sanjian) is a acupoint of the large intestine meridian, which is effective in treating rumbling sound in the stomach and diarrhea9. ST34 (梁丘, Liangqiu) is stomach meridian’s cleft point and is effective in treating abdominal bloating and diarrhea15. Herbal medicine treatment was maintained as it was for the treatment of perforation.
Abdominal pain that the patient complained of from the first visit was NRS 5. It was intermittent with a squeezing, primarily manifesting around the umbilical and right lumbar regions among the nine regions of abdominal area. NRS score decreased to NRS 1-2 on last day of first inpatient treatment period. and there were no complaints of aggravated abdominal pain due to perforation during outpatient treatment from April 9th, 2022 to May 18th, 2022. At this time, there were no additional injections or western medicine prescribed for treating fisutla. NRS 1 level was maintained even at the end of treatment. Also, the frequency of diarrhea decreased from 20 to 13 times per day during treatment. The increase in abdominal pain and inflammatory markers during the early stages of the second hospitalization is presumed to be due to the less proactive treatment and inadequate lifestyle management compared to the inpatient period during the outpatient treatment period.
There were no symptoms such as nausea or chills, related to perforation, and there was no persistent fever. In addition, when we periodically conducted physical abdominal examination, no additional instances of rebound tenderness were observed. WBC, which can be confirmed as inflammatory markers, were detected during the treatment period. There was no significant change in the values within the normal range, so there was no possibility of inflammation. On an abdominal CT taken in May 2022, there was no evidence of inflammation, and it was confirmed that the fistula site had disappeared.
In addition, hepatotoxicity and nephrotoxicity due to Korean medicine treatment were not observed in the blood tests performed in this hospital, and side effects such as pruritus and pain caused by acupuncture were also not found.
If the intestinal perforation is left for a long time, it may cause acute abdominal pain or progressive abdominal pain depending on the location of the occurrence. It is also one of the emergency diseases that require surgery because it can cause complications such as peritonitis. In this case, perforation of the intestine was found during follow-up after total colectomy. With Korean medicine alone, there were no complications or worsening until now, and the patient’s symptoms improved without aggravation due to the perforation. In addition, it was found to show improvement in radiology. Since then, there have been no recurrences of the perforation confirmed on the CT scan, and the symptoms related to the perforation have remained improved.
This case corresponds to the treatment report of one patient, and it has limitations in that some digestive symptoms occurred due to the occurrence of ileus during treatment. In addition, it is suggested that further safety assessments, such as imaging studies like CT scans, should have been conducted for intermediate progress monitoring and the detection of complications in addtion to blood tests and physical abdominal examination. However, through this case, it can be concluded that oriental herbal treatment alone can prevent complications and effectively treat perforation in patients with intestinal perforation without surgical treatment or antibiotic treatment, and additional case reports and large-scale studies are needed in the future.